SURVIVAL AND PUBLIC INTERVENTION RATES
Starting in January 2011, the District of Columbia Fire and Emergency Medical Services Department (DCFEMS) began submitting cardiac arrest data to the Cardiac Arrest Registry to Enhance Survival (or CARES, please click here to view registry website). CARES was developed to help communities determine standard outcome measures for out-of-hospital cardiac arrest (OHCA) locally allowing for quality improvement efforts and benchmarking capability to improve care and increase survival. The CARES registry includes more than 100 data field elements completely describing each cardiac arrest case. DCFEMS is responsible for creating each record and entering most data elements, while hospitals receiving cardiac arrest patients transported by DCFEMS are responsible for entering outcome data elements. During the period of a year, FEMS typically treats and/or transports between 700 and 1,100 cardiac arrest patients.
CARES produces cardiac arrest patient outcome data using “Utstein Style” reports (to view the 2015 AHA statement concerning “Utstein Style” reporting published in a medical journal, please click here). “Utstein Style” reports categorize cardiac arrest patient outcomes using several sorting methods, standardized for nationally comparable data. CARES/DCFEMS “Utstein Style” reports for cardiac arrest patient outcomes by fiscal year (October to September) are available below:
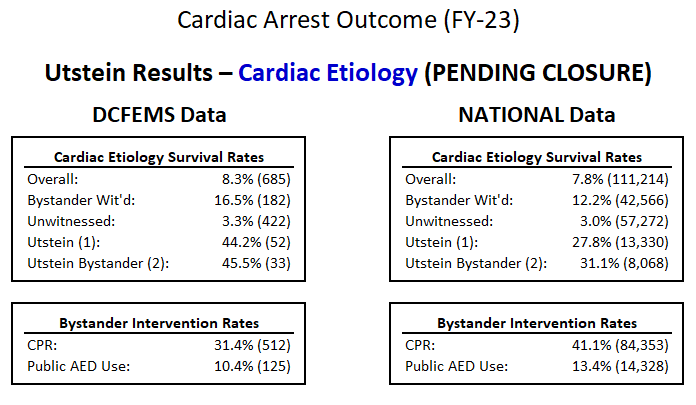
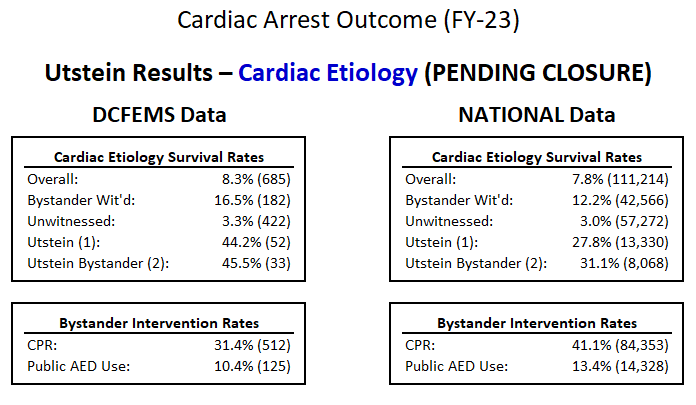
Starting in October 2020 (FY 2021), DCFEMS changed cardiac arrest reporting format to more closely align with CARES “Utstein Style” reports. This change eliminated previously reported measures and now reflects table data shown in “Utstein Style” reports created by CARES. The FY 2021 (and forward) measures include cardiac arrest survival rates for cardiac etiology cases, and bystander intervention rates for CPR and AED use. The table below shows most recent fiscal year data (pending closure means CARES has not completed and updated all agency and hospital data, which occurs each January for the previous year).
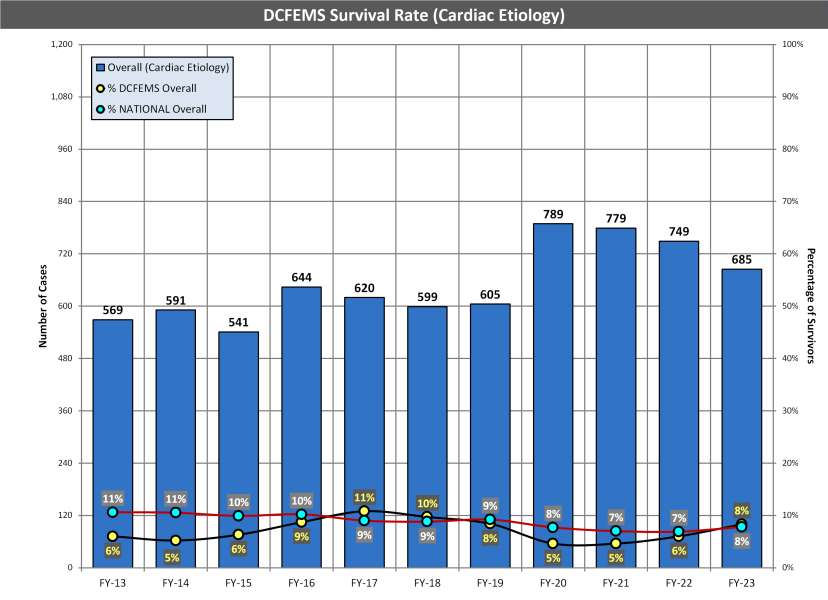
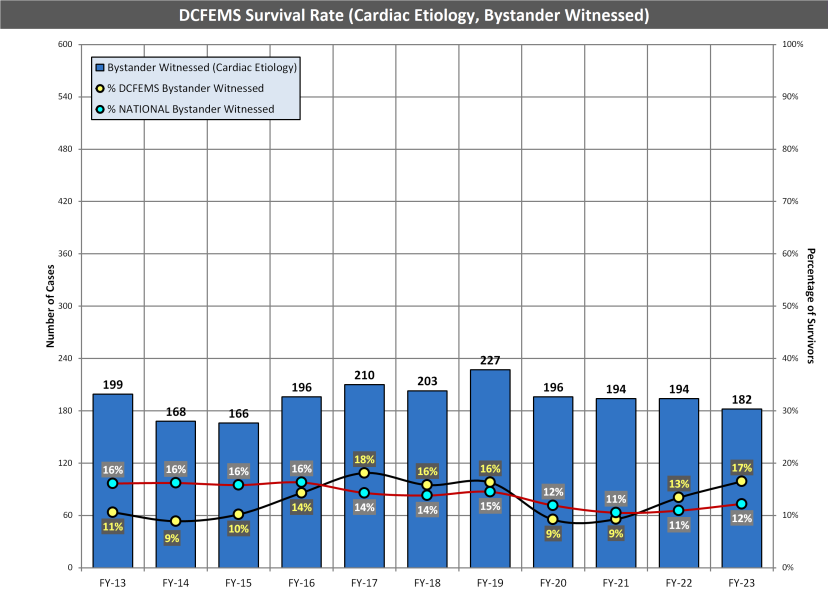
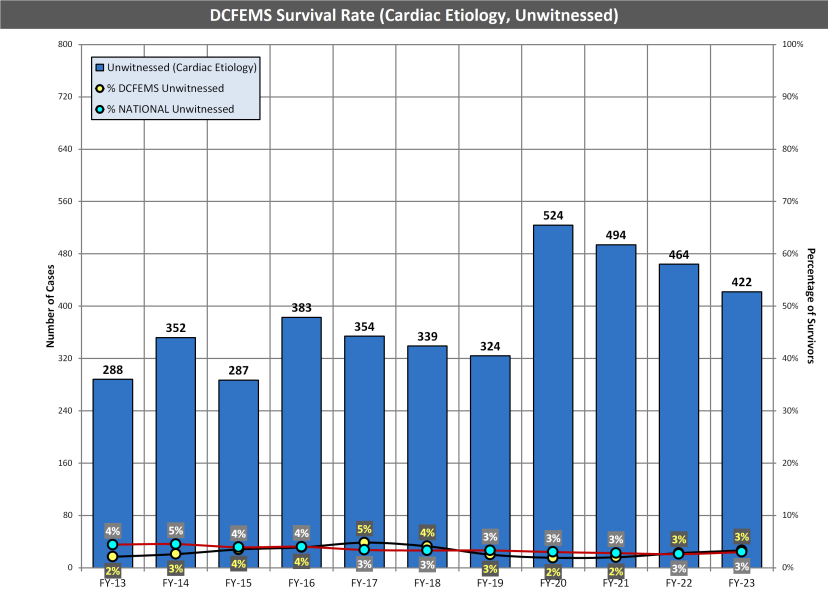
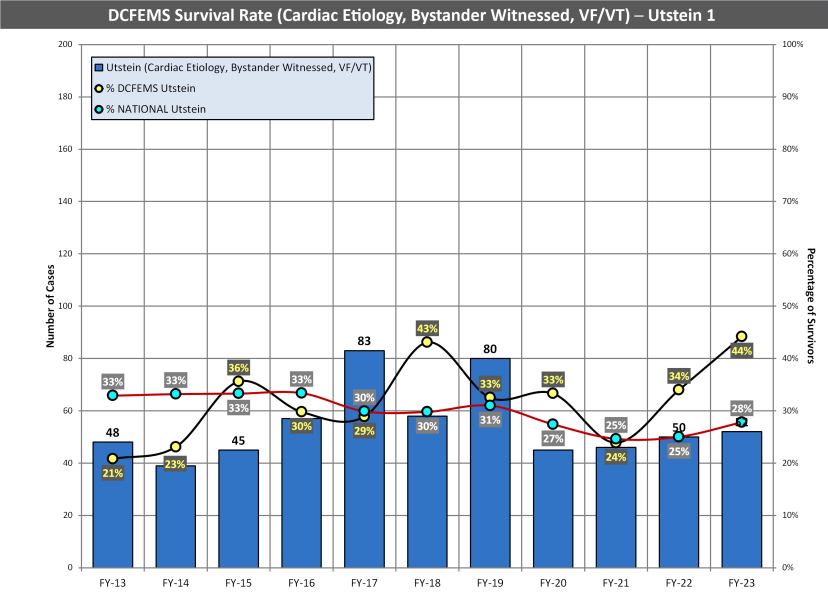
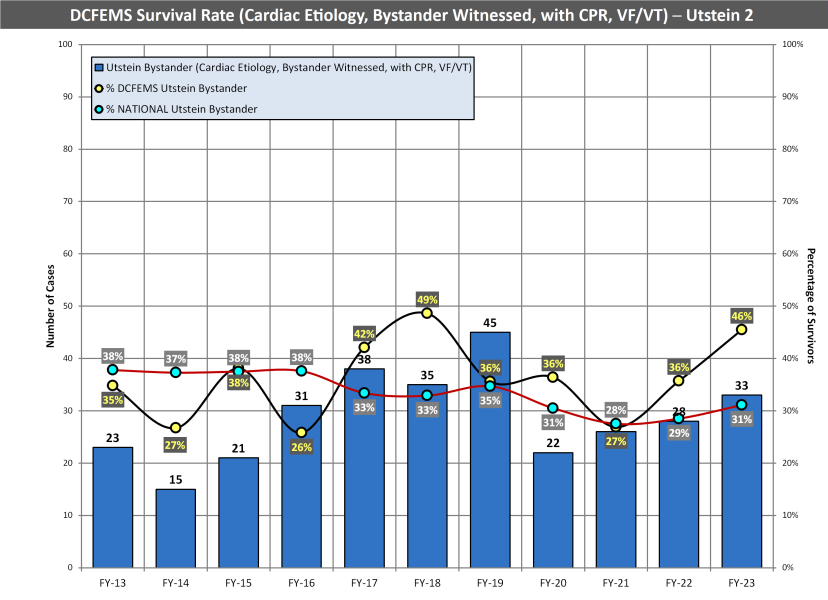
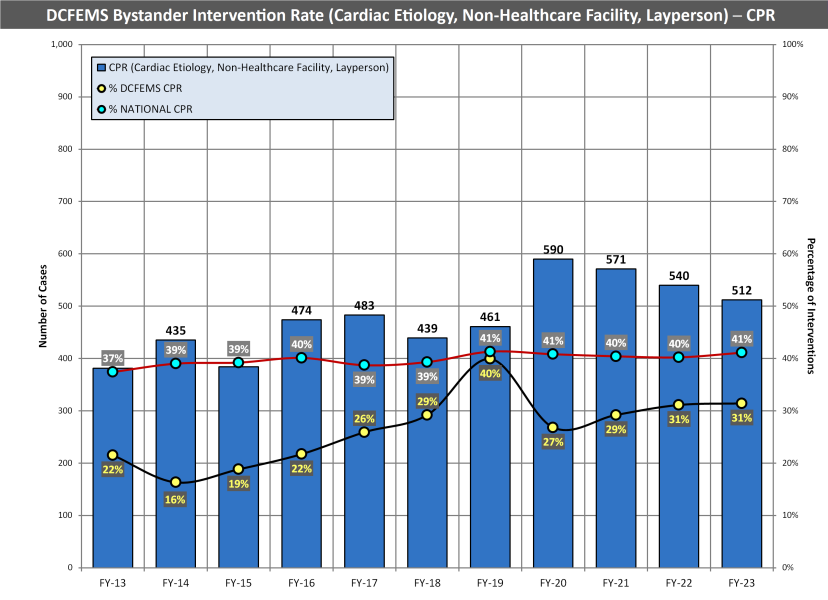
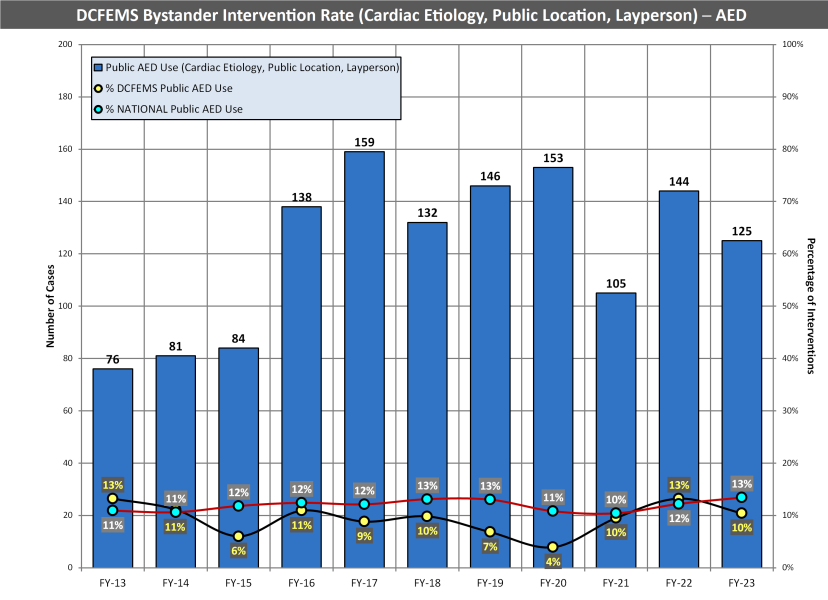
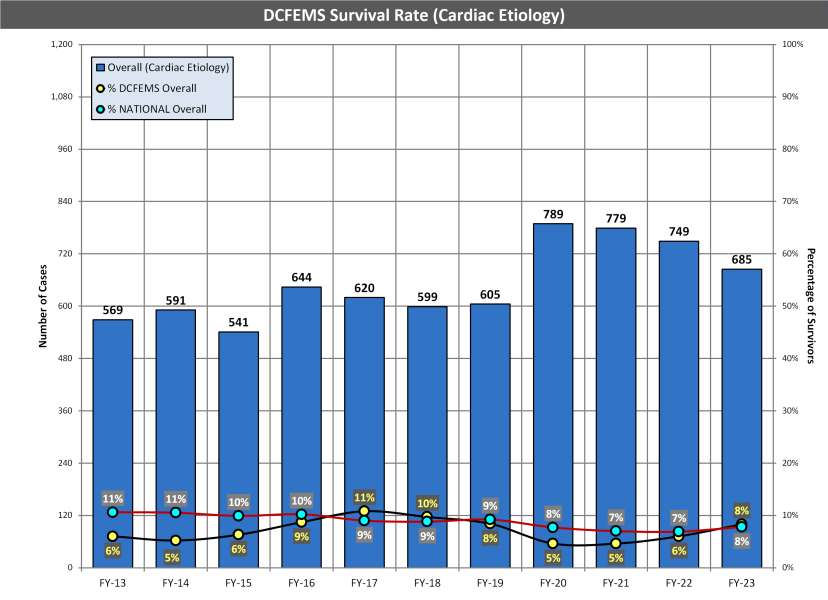
FY 2021 (and forward) measures are presented below and include a ten-year history for each measure. Blue bars are the number of DCFEMS cardiac arrest cases. Black lines with yellow percentages are the DCFEMS measures. Red lines with white percentages are the CARES reported national measures.
• Overall Survival Rate – this cardiac arrest survival rate is calculated by dividing the number of patients “discharged alive” from hospitals by the total number of cardiac arrest cases, both presenting with “cardiac etiology” (for example, myocardial infarction, arrhythmia, and other identified factors).
• Bystander Witnessed Survival Rate – this cardiac arrest survival rate is calculated by dividing the number of patients “discharged alive” from hospitals by the total number of cardiac arrest cases, both presenting with “cardiac etiology” and witnessed by a bystander (excluding 9-1-1 responders).
• Unwitnessed Survival Rate – this cardiac arrest survival rate is calculated by dividing the number of patients “discharged alive” from hospitals by the total number of cardiac arrest cases, both presenting with “cardiac etiology” but NOT witnessed by a bystander.
• Utstein (1) Survival Rate – this is the commonly compared “cardiac arrest survival rate” calculated by dividing the number of patients “discharged alive” from hospitals by the total number of cardiac arrest cases, both presenting with “cardiac etiology,” an “initial rhythm of ventricular fibrillation or ventricular tachycardia,” and witnessed by a bystander (excluding 9-1-1 responders).
• Utstein Bystander (2) Survival Rate – this cardiac arrest survival rate is calculated by dividing the number of patients “discharged alive” from hospitals by the total number of cardiac arrest cases, both presenting with “cardiac etiology,” an “initial rhythm of ventricular fibrillation or ventricular tachycardia,” witnessed by a bystander (other than 9-1-1 responders), AND when CPR and/or AED use was provided by “a lay person, lay person family member or lay person medical provider” (excluding 9-1-1 responders).
• Bystander CPR Intervention Rate – this public intervention rate is calculated by dividing the number of patients in cardiac arrest who received CPR from “a lay person, lay person family member or lay person medical provider” (other than 9-1-1 responders) by the total number of cardiac arrest cases presenting with “cardiac etiology,” NOT occurring in a “nursing home” or “healthcare facility,” and NOT occurring after arrival of 9-1-1 responders.
• Public AED Intervention Rate – this public intervention rate is calculated by dividing the number of patients in cardiac arrest when an AED was applied by “a lay person, lay person family member or lay person medical provider” (other than 9-1-1 responders) by the total number of cardiac arrest cases presenting with “cardiac etiology,” NOT occurring in a “home/residence,” “nursing home” or “healthcare facility,” and NOT occurring after arrival of 9-1-1 responders.