EMS CARE METRICS - CONTINUOUS QUALITY IMPROVEMENT (CQI)
Starting in FY 2020, the DC Fire and Emergency Medical Services Department (FEMS) began adopting the National EMS Quality Alliance (NEMSQA) “Compass 2.0” measures (Compass Measures) as Key Performance Indicators to monitor and evaluate the clinical performance of the Agency (to view information about NEMSQA measures, please click here). The Compass measures were developed by a Technical Expert Panel comprised of medical professionals and subject matter experts to evaluate available science and literature on specific areas of interest in prehospital medicine. When evidence was not available, the Technical Expert Panel relied on subject matter experts and assessed industry practices to determine the value of a particular measure. Additionally, Compass Measures use National EMS Information Systems (NEMSIS) data elements to standardize measures, and subsequently have the added benefit of local, regional, and national benchmarking. These efforts are contributing to the continued success of our emergency medical services through a systematic process of review, analysis and improvement.
The National EMS Quality Alliance patient care metrics:
-
Hypoglycemia – 01: Treatment Administered for Hypoglycemia
-
Pediatrics – 01: Pediatric Respiratory Assessment
-
Pediatrics – 02: Administration of Beta Agonist for Pediatric Asthma
-
Pediatrics – 03: Documentation of Estimated Weight in Kilograms
-
Seizure-02: Patients with Status Epilepticus Receiving Intervention
-
Stroke-01: Suspected Stroke Receiving Prehospital Stroke Assessment
-
Trauma-01: Pain Assessment of Injured Patients
-
Trauma-03: Effectiveness of Pain Management for Injured Patients
-
Trauma-04: Trauma Patients Transported to a Trauma Center
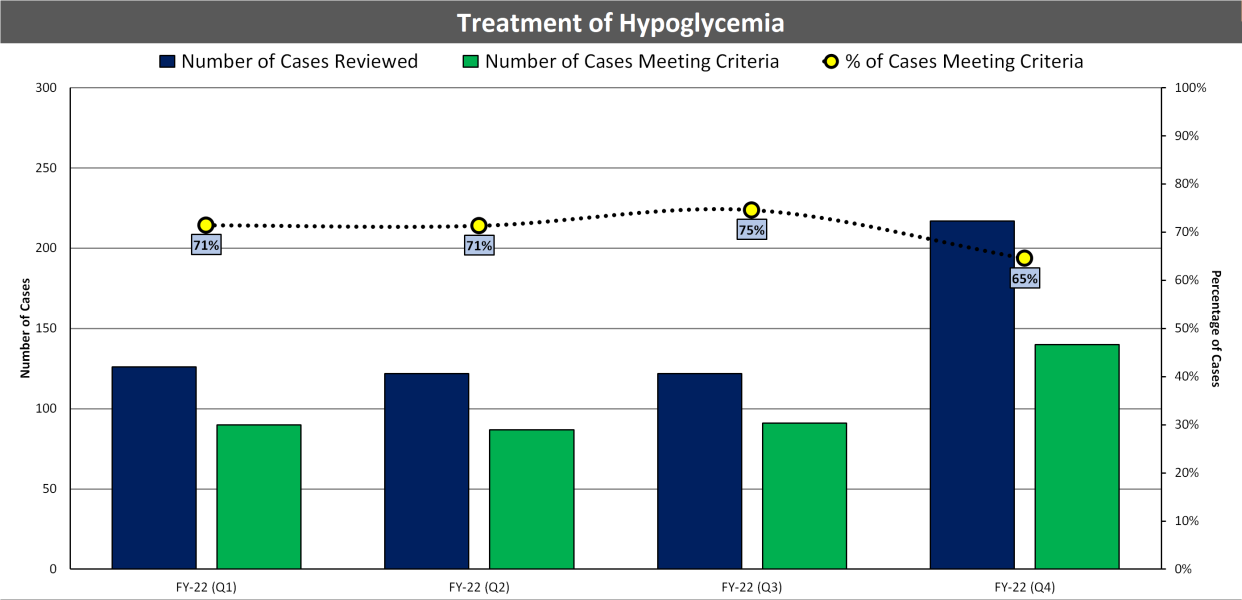
Hypoglycemia – 01: Treatment Administered for Hypoglycemia
Direct evidence for treating hypoglycemia/low blood sugar in the EMS environment is not available. However, it is clearly the standard of care for patients who have the condition. The medical community/literature understands that untreated hypoglycemia can cause brain injury, coma, and other consequences. The intent of this measure is to determine if treatment is being administered to EMS patients who are experiencing hypoglycemia.
Patients that suffer a low-blood sugar event often present with a decreased level of conscious, appear and act intoxicated, or mimic stroke like symptoms. As such, this patient population can be challenging for medical providers if they do not consider low-blood sugar to be an underlying cause for the acute changes. This measure demonstrates the ability of FEMS EMTs and Paramedics to correctly identify a low-blood sugar event and treat the condition accordingly.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):
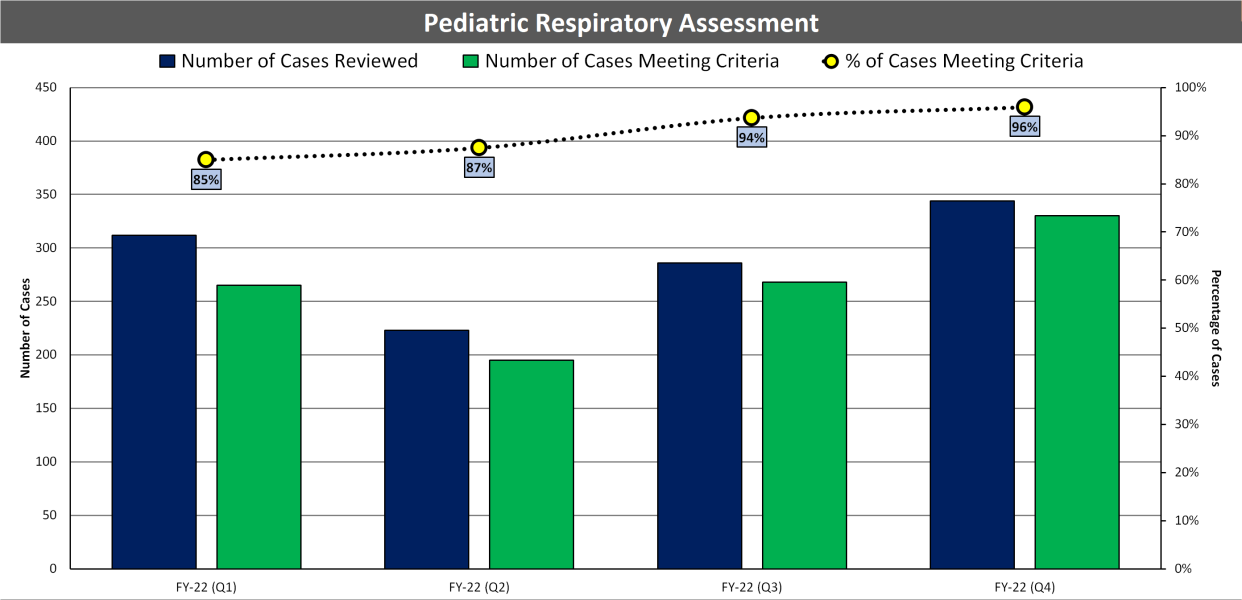
Pediatrics – 01: Pediatric Respiratory Assessment
This measure does not have direct evidence to support its validity. However, it is known that providers often express discomfort with assessment of children and that respiratory distress is one of the most common serious conditions encountered by EMS providers in pediatric patients. The medical community agrees that, if a pediatric patient is experiencing respiratory distress, a respiratory assessment should be performed. Performing a respiratory assessment of a patient is the first step to determining if additional clinical interventions are necessary, and it is important that this process in care be measured. The intent of this measure is to determine if pediatric patients experiencing respiratory distress are receiving respiratory assessments.
The inclusion criteria are for patients less than 18 years of age and has been expanded to include a general impression of respiratory distress, which could include many different respiratory conditions. These changes mirror what is found in current published guidelines and literature for pediatric respiratory distress and assessments.
To the experienced EMS Professional, Pediatrics-01 appears to state the obvious – every patient should have an assessment of their respiratory status. However, documentation of this fundamental element of care is often not completed. This may be simply a documentation omission but may also represent an incomplete clinical assessment or perhaps because providers are less comfortable assessing children than adults. FEMS uses this measure to identify gaps in standard care or documentation of that care, and target areas for improvement.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):
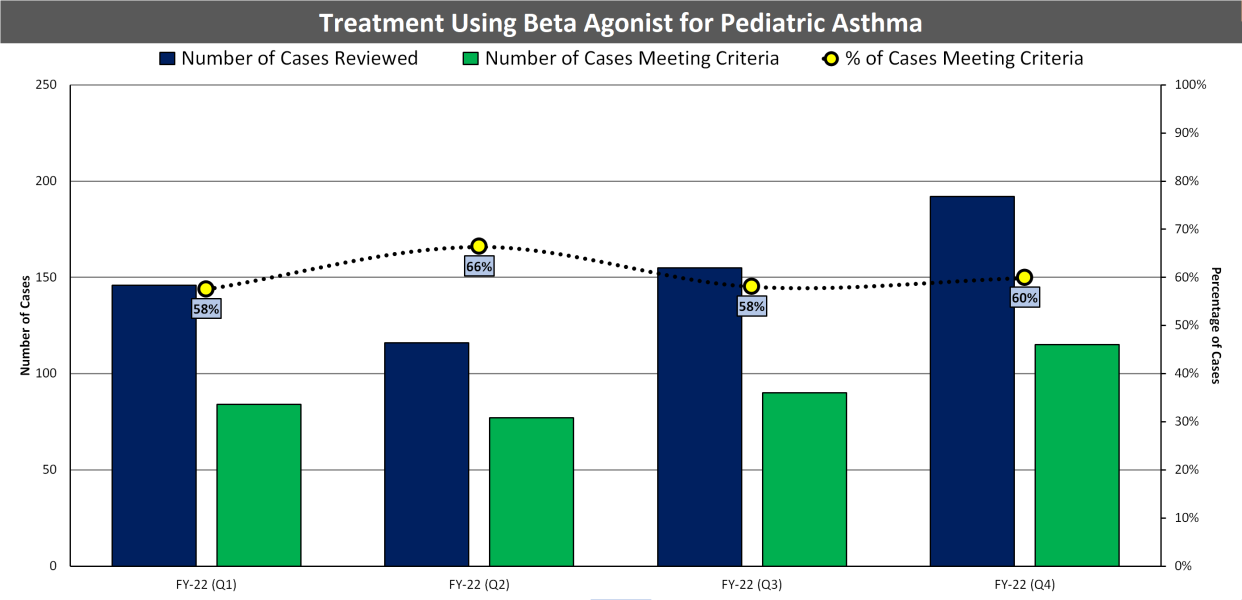
Pediatrics – 02: Administration of Beta Agonist for Pediatric Asthma
Asthma is a common disease among both children and adults, and a common reason for EMS calls. There is strong evidence demonstrating the benefits of albuterol administration to patients with an acute asthma exacerbation in the Emergency Department setting based on patient centered outcomes. There is also evidence to support it can be safely and effectively administered by EMS. There are also national guidelines that support this measure. The intent of this measure is to determine if pediatric patients experiencing asthma exacerbation are receiving a beta agonist.
Pediatrics-02 is a true quality measure, as improvement can be driven by EMS providers themselves. Every State and Region will have variation with regard to availability of Advanced Life Support, Basic Life Support and First Responders as well as protocols for care of pediatric patients with asthma. FEMS considers this a patient-centric measure, meaning treatment can be delivered by both Basic Life Support and Advanced Life Support personnel.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):
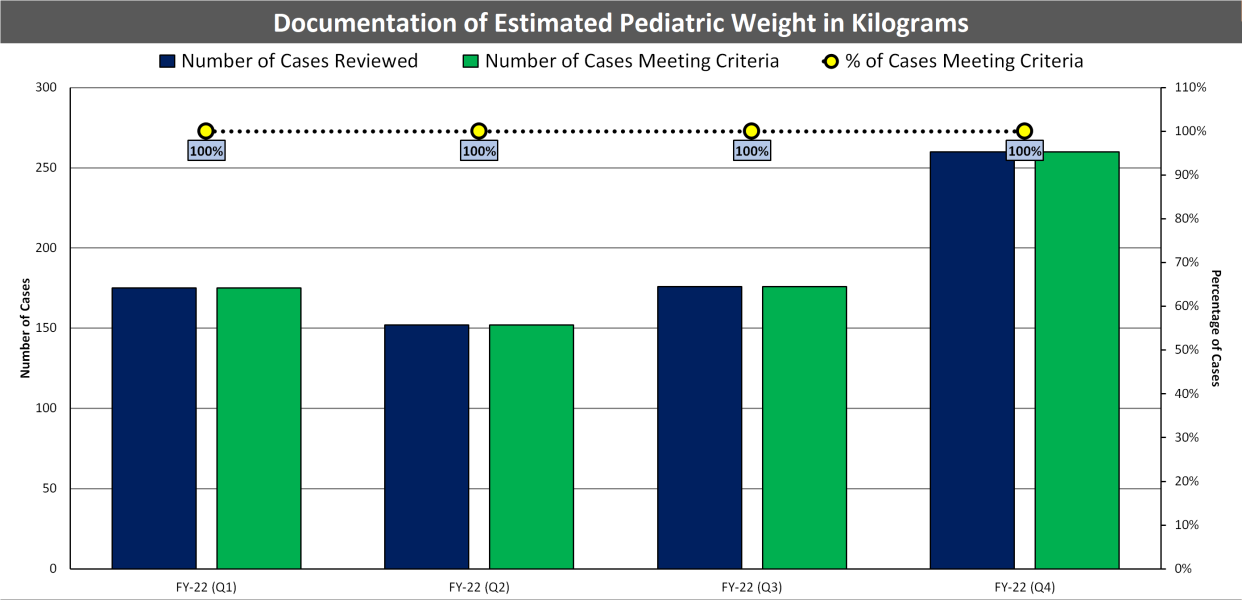
Pediatrics – 03: Documentation of Estimated Weight in Kilograms
Pediatrics-03 is classified as a pediatrics measure in the EMS Compass 2.0 Measure Set, but its intent is deeply rooted in safety. There is significant published literature that attributes pediatric medication errors to errors in converting pounds to kilograms while dosing a medication. With pounds and kilograms commonly being confused, leading to pediatric medication errors, Pediatrics-03 is important for measuring a clinical documentation process that can lead to better patient outcomes. The intent of Pediatrics-03 is to determine if the weight of EMS pediatric patients is being documented in kilograms.
Pediatric patients make up approximately 5-10% of patients taken care of by EMS. Critical pediatric patients make up < 1 percent of these patients. The accurate dosing of many medications to pediatric patients requires calculation based on the patient’s weight in kilograms. In these rare high stress situations, the likelihood of making a medication error on a pediatric patient is high even when the weight is measured and documented appropriately. Measuring this specific population will drive FEMS to consider how the Agency is performing this critical task and how they can improve. This will, in turn, lead to a system that will have higher likelihood of providing the correct dose to a patient thereby improving the safety of medication administration.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):
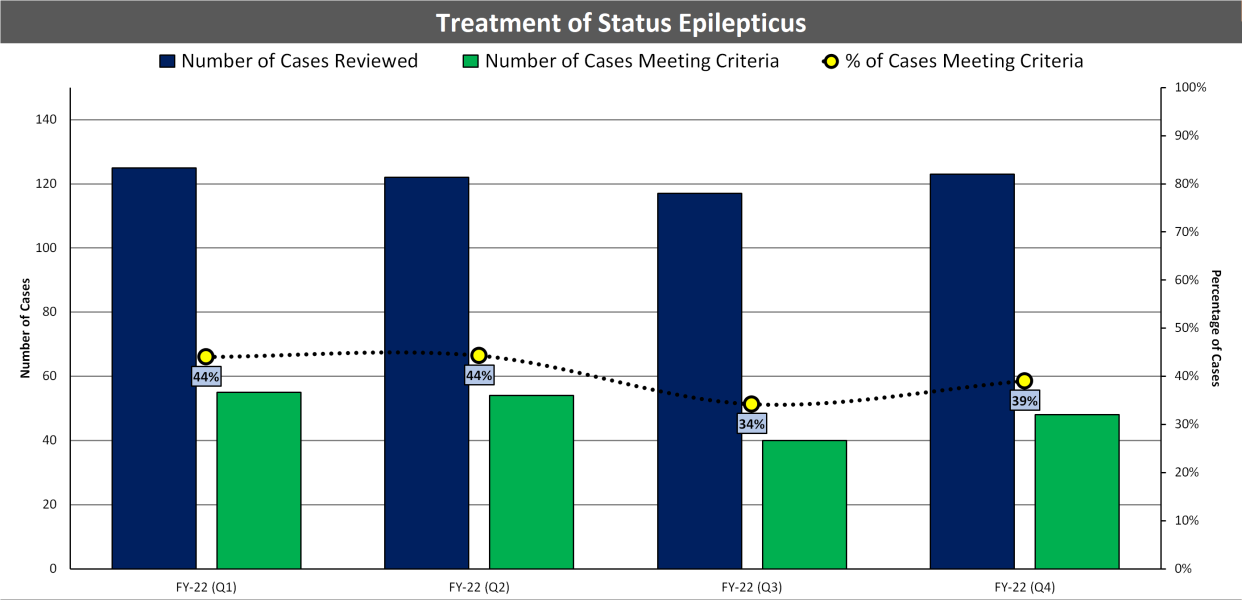
Seizure-02: Patients with Status Epilepticus Receiving Intervention
EMS is commonly faced with caring for patients with status epilepticus. The published rationale and guidelines support this measure – patients experiencing status epilepticus utilize EMS for care and the efficacy of treatments (e.g., benzodiazepines) is evident. There is also strong evidence that earlier of treatment of status epilepticus results in improved patient outcomes. D.C. Fire and EMS uses this indicator with the intent of measuring whether or not patients with status epilepticus are receiving benzodiazepines.
EMS systems have the opportunity to provide well evidenced benefit to patients by initiating prehospital treatment of status epilepticus. EMS agencies and systems can use this measure to establish how often they are providing this potentially lifesaving therapy. If variability in care or areas for improvement are identified quality improvement efforts can be targeted for this group of patients.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):
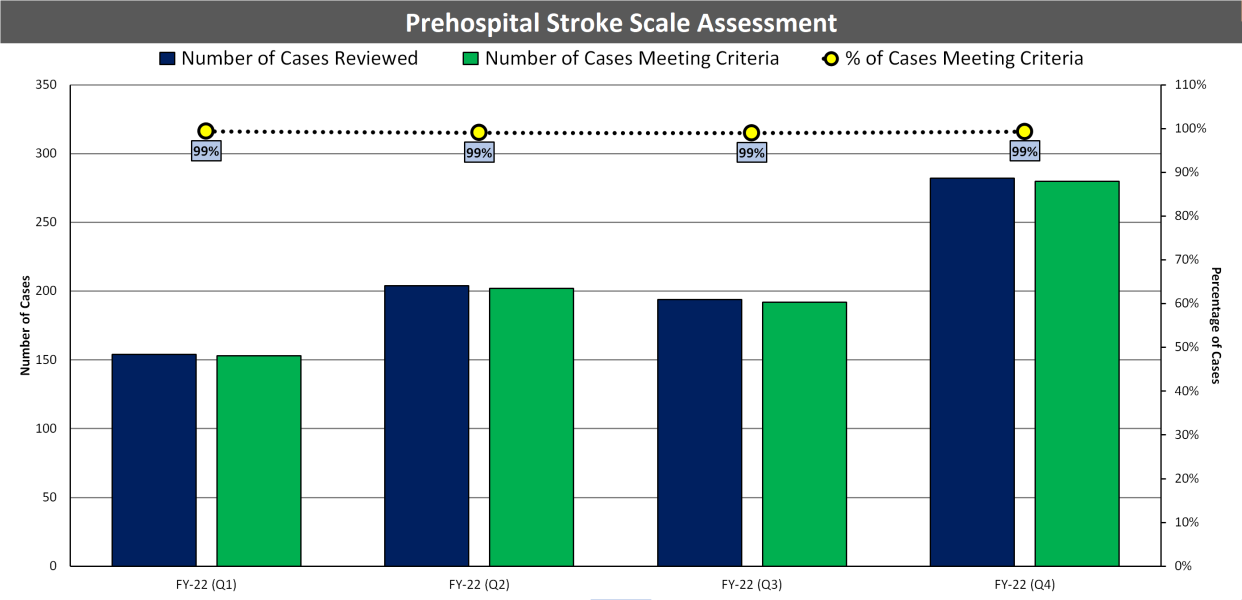
Stroke-01: Suspected Stroke Receiving Prehospital Stroke Assessment
While the direction of published evidence can vary for prehospital stroke scales, it is widely understood that stroke assessments are helpful tools in helping identify patients with stroke and determining which facilities are most appropriate for their transport. The intent of this measure is to determine how many suspected stroke patients are receiving prehospital stroke assessments (and having the assessment documented), on scene during the EMS encounter.
As Stroke Systems of Care become more robust across the country and EMS becomes an increasingly important partner in identifying stroke, this measure will support a key task of prehospital providers in the care of stroke patients – making the diagnosis and key transport decisions.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):
Trauma-01: Pain Assessment of Injured Patients
EMS has a role in assisting with pain management and it is important that pain is assessed and documented. There is evidence of variability in how often pain is assessed and treated by EM professionals. The intent of this measure is to determine if pain is assessed (and documented) for injured patients who are transported by EMS.
Assessment and treatment of pain in the prehospital environment is an opportunity for EMS to impact an outcome that is highly valued by patients (relief of pain). Published evidence demonstrates that there is wide variability and opportunities for improvement in this area. EMS systems or agencies can use this measure to assess how they are performing and identify areas for quality improvement efforts.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):

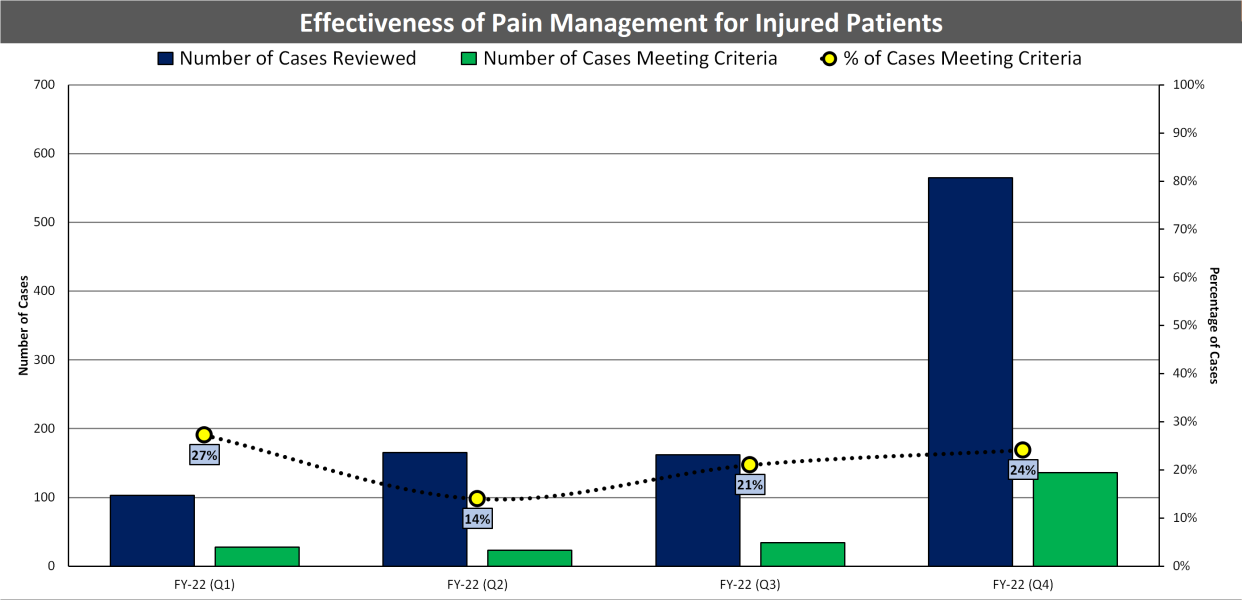
Trauma-03: Effectiveness of Pain Management for Injured Patients
Trauma-03, is an outcome measure that measures the effectiveness of pain management for injured patients who are transported by EMS. The published evidence supporting this measure is similar to that of Trauma-01, as EMS often treats patients with pain and there are many clinical indicators for pain management. The intent of this measure is to determine if pain is being reduced for EMS patients during the EMS encounter. The true intent of this measure is to determine if EMS providers are helping their injured patients feel better, not if they are administering opioids to their patients.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):
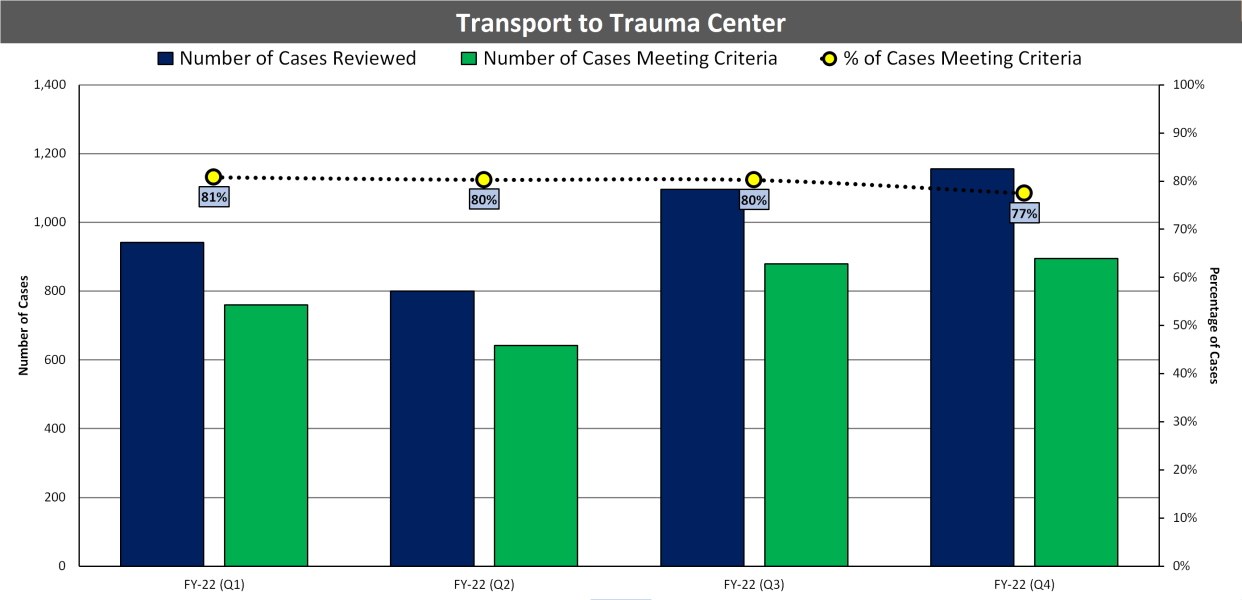
Trauma-04: Trauma Patients Transported to the Trauma Center
Trauma-04 was designed using CDC guidelines for Field Triage of Trauma Patients. Along with the CDC guidelines, published literature clearly supports this measure, as patients who receive appropriate trauma care often have better outcomes.
As a metropolitan area, the District of Columbia benefits from multiple Trauma Centers, including Children’s National Hospital Center which specializes in pediatric trauma. Given the accessibility to these facilities, DC FEMS seeks to achieve high compliance rates with this measure.
The chart below shows the number of required patient cases reviewed, with the number and percentage of the cases meeting the required criteria by FEMS personnel for Fiscal Year 2022 (by fiscal year quarter):